1.0 Introduction.
Diabetes mellitus (DM) is a group of metabolically associated disorders of diverse etiologies characterized by sustained elevation of blood glucose due to defects in the secretion of insulin or its action. Thus, it is often associated with disturbances in the metabolism of carbohydrate, protein and fat [1]. Hyperglycemia is a random blood glucose level above or equal 11.1mmol/l (200 mg/dl) or fasting plasma glucose level above or equal 7.0 mmol/l (126 mg/dl) and it leads to long-term damage, dysfunction, and failure of different organs, especially the eyes, kidneys, nerves, heart, and blood vessels [2]. Diabetes mellitus may also result from a complex interaction between environmental and genetic factors.
Based on the etiology of DM, factors which contribute to hyperglycemia are reduction in the secretion of insulin, a reduction in glucose utilization, and a rise in the synthesis of glucose [2]. Diabetes mellitus associated metabolic alterations give rise to secondary pathophysiological changes in many tissues, thus imposing considerable burden on both DM patients and the health care system [2]. Calcium is one of the body’s mineral cations, it is obtained majorly through dietary intake of milk products such as yoghurt, cheese and butter, foods fortified or supplemented with calcium and leafy vegetables that are dark green in color [3].
Serum calcium is important for several cellular processes that undergo tight regulation which includes absorption of intestinal calcium, turnover of bone reabsorption and filtering of the kidneys [4]. Serum calcium constitutes about 1% of total body calcium, its functions include contraction of muscle, constriction, and dilatation of the vascular system. The listed functions are important in catabolism of cholesterol, regulating blood pressure and secretion of insulin, which are crucial causes of metabolic syndrome hypertension, and diabetes [5]. Serum calcium, together with the regulatory endogenous factors and their receptors which include hormone of the parathyroid gland, vitamin D, parathyroid hormone related peptide, Ca2+ and kidney function which regulate its cellular processes have been linked with alterations in the metabolism of glucose—which impairs function of beta cells of the pancreas or sensitivity of insulin thereby increasing the risk of diabetes mellitus. However, the exact mechanism by which serum calcium may relate to diabetes risk is still unclear [4]. The link between increased risk of diabetes and serum calcium levels is complex, decipherment of this link may present a novel opportunity to fight the diabetes epidemic.
Calcium functions not only in the mineralization of the skeletal system but other various cellular functions [6]. Diabetes Mellitus is implicated in the association between impaired bone turnover and absorption of calcium from the intestine, therefore, causing derangements in calcium metabolism [7]. Serum calcium in relation to bone health has been studied widely; however, some epidemiologic studies have shown a positive relationship between increased serum calcium levels and DM [3]. Another study done by [5] also showed that high serum calcium is associated with diabetes mellitus. Also, Zhu et al., [8] relating calcium levels and diabetes mellitus showed that high calcium levels in serum are associated with risk of type 2 DM. However, these epidemiological studies seem to be inconsistent as some studies show a decrease in serum calcium concentration in people with type 2 DM such as this research which was done in a teaching hospital in Nigeria [9]. The reason to the inconsistency in some of these studies as reviewed by Zhu et al. [8] may be partially explained by the different ways of measuring serum calcium such as total serum albumin-corrected serum, serum ionised or plasma levels or heterogeneous study populations with various outcomes.
The aim of this study was to evaluate the serum calcium levels in patients with T2DM and to determine any correlation between serum calcium levels, clinical features of DM patients and their HbA1c levels.
2.0 Materials and Methods
2.1 Study area
This study was conducted in the Endocrinology unit of the University of Calabar Teaching Hospital (UCTH) in Calabar Municipal Local Government Area of Calabar Cross River State, Nigeria. Calabar is the capital of Cross River state which is located in the South- South geopolitical zone of the country. The University Teaching Hospital where the study was conducted receives referrals from the general hospitals and other peripheral health facilities within Calabar and elsewhere within the state. The Endocrinology clinic of the hospital attends to patients on a weekly basis. Diabetic patients constitute a large proportion of attendees in this clinic. Services are provided by specialist endocrinologists, resident doctors in training and nurses.
2.2 Study population
Study subjects were diabetic patients receiving care from the Endocrinology clinic of the University of Calabar Teaching Hospital (UCTH) while the controls were relatives of patients and administrative staff of the hospital.
2.3 Inclusion and exclusion Criteria
Diabetic patients 18 years and above who consented to participate in the study were selected for this study after carefully explaining the aim and procedures of the study. The following set of patients was excluded from the study:
- Patients on thiazide diuretics: This is because thiazide diuretics enhance calcium reabsorption in the distal convoluted tubule and can therefore cause hypocalcaemia.
- Patients with proteinuria of ≥ 2+: Calcium is normally bound to albumin; results will be altered if there is proteinuria as this can cause hypoalbuminaemia.
- Patients with chronic kidney disease/ or diabetic nephropathy: In this condition, patients have proteinuria which can cause hypoalbuminemia leading to hypocalcemia.

Figure 1; Map of Calabar Municipal (10)
2.4 Study design
This study was a comparative case control study, in which a total number of one hundred and twenty-six patients participated; Systematic sampling technique modelled after the method of Nwankwor et al. (9) was used in the selection of cases. A total number of 300 diabetic patients are contained in the clinic register. The calculated sample size for this study is approximately 63. The sampling fraction was generated by dividing the total population by the calculated sample size.
Sampling fraction=Study population/calculated sample size.
=300/63 =4.76≈5
Therefore, every fifth person who gave informed consent was included in the study until the sample size was reached. However, the first participant was selected by balloting. Diabetic clinic sees patients every Wednesday of the week, about 20 patients are seen, therefore 20 pieces of paper were cut into equal sizes and then serially numbered from 1-20. These papers were put into a container and shuffled and one was randomly selected and this yielded the number 5. The first participant to be selected was the 5th patient seen after whom every 5th subject who gave informed consent was selected for the study. This was done over a 12-week period.
Healthy controls were selected amongst relatives of selected patients and relatives of other patients (not participating in the study) seen in the clinic who were not diabetic. To make up for the deficit in sample size, hospital staff was also selected with their consent. Permission was sought from the Ethical Review Committee of the University of Calabar Teaching Hospital, Calabar.
2.5 Data Collection
Data was collected using a questionnaire and this questionnaire was administered by trained Research Assistants. The questionnaire was divided into different sections as shown below.
Section A: Socio-Demographic Data: hospital number, age, sex, ethnic group, marital status, monthly income after tax, religion, highest educational level, occupation, address.
Section B: medical history, lifestyle, and co-morbid conditions.
2.6 Blood Collection
From each patient, 2 millilitres (ml) of venous blood was collected from the antecubital veins using vacutainer needles and bottles. Blood was transferred to EDTA tubes for HbA1c estimation and was stored at -4 0C before analysis. Blood samples for calcium and albumin were centrifuged at a rate of 3000rpm/10minutes and transported on dry ice and stored at 20 0C until analysed [9]. Fasting blood glucose was estimated with the aid of Accu-Chek Active® glucometers and test strips which uses the hexokinase method for glucose estimation, with results comparable to blood glucose concentrations in venous plasma as recommended by the International Federation of Clinical Chemistry and Laboratory Medicine [9].
2.7 Biochemical Assays
Estimation of Plasma Total Calcium was carried out using the standard colorimetric assay method, HbA1c estimation was done using ion-exchange chromatographic – spectrophotometric method while Plasma albumin concentration was measured using the Colorimetric Bromocresol Green (BCG) method. The estimation of albumin adjusted calcium was also estimated [11].
2.8 Statistical Analysis
Statistical analysis of data collected was done using SPSS version 20.0 (IBM, Armonk New York, USA).
3.0 Results
3.1 Social characteristics of type 2 DM patients (Sex, Age, Marital Status, Occupation and Religion)
There were altogether 126 participants in the study; 63 were diabetics and 63 were non-diabetics. There were more females (58.7%) than males (41.3%) in the study sample. Most of the participants were married (74.6%), and an equal proportion was either self-employed or public/civil servants. All participants except one were Christians (Table 1). The mean age of diabetic participants (54±11.7years) was increased compared with the mean age for non-diabetic (40.0±10.5years) (p<0.009). A greater percentage of diabetic subjects were females 42(66.7%), married 52 (82.5%), self-employed 28 (50.9%). For the non-diabetic participants, about 50.8% (n=32) were females, 66.7% (n=42) were married and 54.1% (n=33%) were civil/public servants (Table 1).
Table 1: The social demographics of type 2 DM patients enrolled in the study
| Variables | Category | Diabetic status | ||||
| Diabetics | Non-diabetics | Totals | ||||
| N | % | N | % | N(%) | ||
| Sex | F | 42 | 66.7 | 32 | 50.8 | 74(58.7) |
| M | 21 | 33.3 | 31 | 49.2 | 52(41.3) | |
| Age* | 63 | 54.0(11.7) | 63 | 40.0(10.5) | – | |
| Marital status | Married | 52 | 82.5 | 42 | 66.7 | 94(74.6) |
| Others | 11 | 17.5 | 21 | 33.3 | 32(25.4) | |
| Occupation | Student/unemployed | 4 | 7.3 | 6 | 9.8 | 10(8.6) |
| Pensioner | 8 | 14.5 | 2 | 3.3 | 10(8.6) | |
| Self-employed | 28 | 50.9 | 20 | 32.8 | 48(41.4) | |
| Civil/public servant | 15 | 27.3 | 33 | 54.1 | 48(41.4) | |
| Religion | Christianity | 62 | 98.4 | 63 | 100 | 125(99.2) |
| Islam | 1 | 1.6 | 0 | 0 | 1(0.8) |
*Mean (standard deviation)
3.2 Comparison of serum calcium ion concentration in diabetic and non diabetic patients
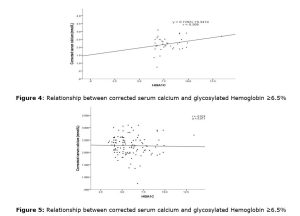
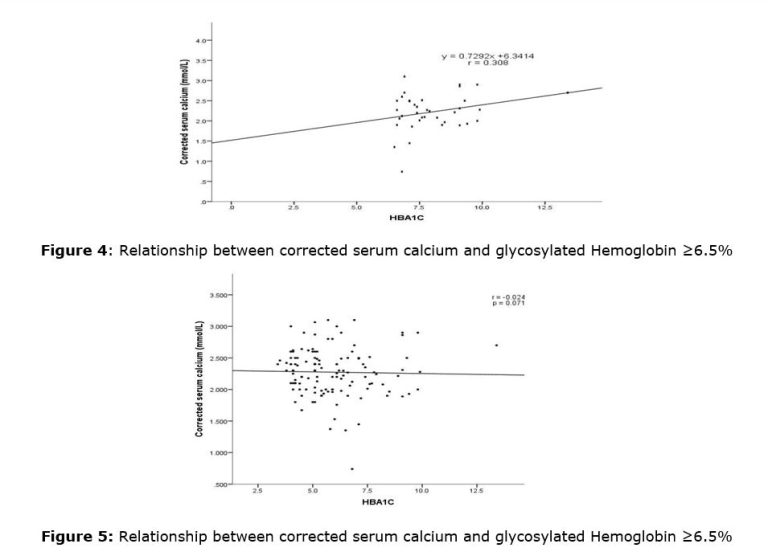
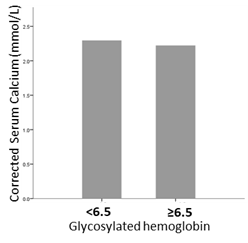
The mean calcium concentration in serum of diabetics and non-diabetics attending clinic in UCTH were 2.33mmol/l±0.04 and 2.22±0.05mmol/l, respectively, and the difference was not statistically significant (t-statistics = 1.662, df = 124, p-value=0.099) (Figure 2). The mean serum calcium in patients with glycosylated haemoglobin lower than 6.5 is slightly higher than mean serum calcium in patients with haemoglobin higher than 6.5 (Figure 3)
3.3 Relationship between Serum Calcium and Blood Glucose Control as Indicated by Glycosylated Haemoglobin
The mean serum calcium when glycosylated haemoglobin values were below 6.5 and above 6.5 are represented in the scattered diagram in figure 4 and 5. There was a positive but non-significant correlation between the concentration of glycosylated haemoglobin and serum calcium in subject with glycosylated haemoglobin levels above 6.5 (Figure 4). However, subjects with glycosylated haemoglobin levels below 6.5 showed negative non-significant correlation between glycosylated haemoglobin concentration and serum calcium levels (Figure 5).


4.0 Discussions
Diabetes mellitus is a diverse group of metabolic disorders which have been associated with notable derangements in multiple organ systems of the body. Diabetes mellitus in addition to causing alterations in the functions of vital organs also causes derangements in metabolism of calcium by impairing the activities of calcium regulating organs, including kidney, bone and intestine. Secretion of insulin as a result of increased concentration of blood sugar is dependent on Ca2+ and defects in secretion and action of insulin are related to type DM, thus an abnormal calcium homeostasis could play an important role in the development of type 2 diabetes [12]. This work explored the relationship of serum calcium levels and diabetes mellitus.
Overall, mean serum calcium levels in diabetics and non-diabetics were similar. This supports the work done by [13]. They attributed their findings to relative availability of dietary calcium sources, the multiple origins of serum ALP, and the partially controlled patients’ hyperglycemia. There was no statistically difference between diabetic status and calcium concentration in serum. In the present study sample, the average age of diabetic subjects was higher than the mean age of non-Diabetic subjects (p≤0.05). This is in line with the result of a study by Dahiru et al. [14] who reported that Nigeria in Sub-Saharan Africa has the highest number of people of the adult population aged 20-79 years, with an estimate of 3.9 million living with diabetes mellitus. Additionally, a higher proportion of diabetic subjects were females and self-employed. This agrees with the result of Krishna et al. [15] who reported that a reasonable number of women are becoming increasingly vulnerable to the disease, and existing statistics show that two out of every five women are diabetic and of reproductive age, thus accounting for over 60 million women globally. WHO [16] records over 199 million women living with Diabetes mellitus all over the world and from experts opinion this present figure will increase to 313 million by 2040. The overall mean corrected serum calcium level in the study population was 2.22mmol/L and this was within normal limits. The mean corrected serum calcium level was low in diabetic subjects, supporting the study done by Pittas et al. [17] which reported a significant reduction in the mean serum calcium level of diabetic patients.
Another study done in a teaching hospital in Nigeria by [9] also presented a significant decrease in mean serum calcium of type 2 diabetic patients compared with controls. Thus in this present study, it did not differ from the controls at p ≤ 0.05. The normal range of serum calcium seen in diabetics participating in this study may be due to the fact that these participants were receiving treatment in the Teaching Hospital and consequently, had achieved good blood glucose control. Majority of the diabetic subjects were well controlled as seen by their glycosylated haemoglobin value lower than 6.5. As shown in the study by [7] where PTH –induced stimulation of 1,25 (OH)2D3 production was impaired in diabetic conditions and its production restored with insulin treatment, the result for mean serum calcium level showed that diabetic subjects who had glycosylated haemoglobin (HBA1C) below 6.5 had slightly higher mean serum calcium level than those whose glycosylated haemoglobin was above 6.5.
Although Nagasaka et al. [16], demonstrated that hyperglycaemia leads to increased renal phosphorus and calcium excretion in subjects with type 2 DM, our results do not support this conclusion as no significant difference existed in serum calcium levels of diabetics relative to glycaemic control. Our correlation analyses showed a positive non-significant relationship between corrected serum calcium and glycosylated haemoglobin in diabetics with HbA1c<6.5%, and a contrary relationship in diabetics with Hba1c ≥ 6.5%. In all diabetics, an almost horizontal line of best fit was seen in the regression plot. This tends to support the earlier observation that there was no relationship between serum calcium levels and glycemic control in this study population. The regression analysis did not suggest a relationship between corrected serum calcium and diabetic status despite controlling for a set of socioeconomic variables. There was, thus, no meaningful indication of a negative confounding of the relationship.
5.0 Conclusion
The result shows there is no statistically significant difference between mean serum calcium concentration in diabetic and non-diabetic patients and this may be due to good blood glucose control in these diabetic patients
Conflict of Interest: The author declared no conflict of interest exist
Funding: The study was wholly funded by the authors and no external funding was received
Authors contribution: This work was conducted with the collaboration of all authors: Author IAH, EOO and OHC designed the study, Authors IAH, OYM and EB administered and collated the questionnaires, all authors participated in the clinical and laboratory studies, Author AAR prepared the manuscript. The manuscript was read and approved by all authors.
Acknowledgement: The authors would like to appreciate the HOD and staff of the department of Internal medicine, University of Calabar, the patients who participated in this study; we would also like to acknowledge the staffs of the endocrinology unit of the University of Calabar Teaching Hospital who were of immense assistance throughout the duration of the study.
References
- World Health Organization Definition (1999). diagnosis and classification of Diabetes Mellitus and its complications; report of WHO consultation. (WHO/NCD/NCS/99.2). Part 1: Diagnosis and classification of diabetes mellitus. Geneva: World Health Organization. (1999).
- American Diabetes Association.(2010). Diagnosis and classification of diabetes mellitus [published correction appears in Diabetes Care. 2010 Apr;33(4):e57]. Diabetes Care. ;33 Suppl 1(Suppl 1):S62-S69. Doi: 10.2337/dc10-S062.
- 3.Rooney MR, Pankow JS, Sibley SD, Selvin E, Reis JP, Michos ED, Lutsey PL (2016). Serum calcium and incident type 2 diabetes: the Atherosclerosis Risk in Communities (ARIC) study. American Journal of Clinical Nutrition. 104(4):1023-1029. doi: 10.3945/ajcn.115.130021..
- Chatterjee R. & Lin, P. H. (2016). Serum calcium and its complex association with incident type 2 diabetes. American Journal of Clinical Nutrition,; 104: 957-965
- Chou, C.W., Fang, W. H, Chen, Y. Y., Wang, C.C., Kao, T.W., Wu, C.J and Chen, W.L (2020). Association between Serum calcium and Risk of cardiometabolic disease among community-dwelling adults in Taiwan. Scientific Reports; 10: 3192.
- Peacock, M (2010). Calcium metabolism in health and disease. Clinical Journal of American Society of Nephrology,; 5(1): 23-30.
- Wongdee, K., Teerapornpuntakit, J., Sripong, C. Longkunan, A., Chankamngoen, W and Keadsai, C., Kraidith, K., Krishnamra, N and Charoenphandhu, N (2016). Intestinal mucosal changes and upregulated calcium transporter and FGF-23 expression during lactation: Contribution of lactogenic hormone prolactin. Archives of Biochemistry & Biophysics,; 590: 109-117.
- Zhu J, Xun P, Bae JC, Kim JH, Kim DJ, Yang K, He K. (2019). Circulating calcium levels and the risk of type 2 diabetes: a systematic review and meta-analysis. British Journal of Nutrition. 28;122(4):376-387.
- Nwankwor, H., Nwatu, C., Okwara, C., Young, E.E. Olisaka L.C., Ezomike N.Cand Muoneke U.V (2020). Low serum calcium levels occur in Nigerian adults with type 2 diabetes and correlates negatively with their glycosylated haemoglobin levels: A case-control study. Nigerian Journal of Medicine, 2020; 29(2): 229.
- Harry, Thomas & Etim, Ifiok & Etim, Camillus. (2022). Sedimentology and Palynology Models of Sedimentary Sections Along Lemna Section of The Benin Formation. Pakistan Journal of Geology. 24-28. 10.26480/pjg.01.2022.24.28.
- Gyorgy C (1996). Free hormone measurements, Immunoassay, 423-481, ISBN 9780122147302, https://doi.org/10.1016/B978-012214730-2/50021-2.
- Becerra-Tomás N, Estruch R, Bulló M, Casas R, Díaz-López A, Basora J, Fitó M, Serra-Majem L, Salas-Salvadó J. Increased serum calcium levels and risk of type 2 diabetes in individuals at high cardiovascular risk. Diabetes Care. 2014 Nov;37(11):3084-91.
- Hamad, N. A., Eltayeb, L. B., Brair, S. L., Bakheit, K. H., Hamdan, H. Z., & Omer, W. H. O. A clinical study of serum calcium, phosphorus, and alkaline phosphates level in type II diabetes mellitus among Sudanese population in Khartoum State, 2020; 2012-2013.
- Dahiru, T., Aliyu, A. A. & Shehu, A. U. . A review of population based studies on diabetes mellitus in Nigeria. Sub-Saharan African Journal of Medicine, 2016;3:59-64.
- Krishna, G. S., Bubblu, T. & Amarabalan, R. Role of vitamin D in diabetes. Journal of Endocrinology and Metabolism, 2011; 1(2): 47-56.
- World Health Organisation, World diabetes day. Nhp.gov.in/world-diabetes-day-2017_Pg. (2017).
- Pittas, A. G., Lau, J., Hu, F. B. & Dawson-Hughes, B. The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. Journal of Clinical Endocrinology and Metabolism, 2007; 92(6): 2017-2029
- Nagasaka S, Murakami T, Uchikawa T, Ishikawa SE, Saito T (1995). Effect of glycemic control on calcium and phosphorus handling and parathyroid hormone level in patients with non-insulin-dependent diabetes mellitus. Endocrinology Journal;42(3):377-83.