1.0 Introduction.
Over the recent time, the use of natural and synthetic chemicals has largely created our modern world which has improved the lives of billions of people. Some of these chemicals have been used by the food industry to improve food safety and quality and reduce spoilage and wastage, thus increase its availability, accessibility, and affordability [1,2]. As with any technology, the use of such chemicals are not without certain risks especially in a developing nation which Nigeria is one where international standards and practices like Occupational Safety Health and Administration (OSHA), Registration, Evaluation, Authorization, and Restriction of Chemicals (REACH) and international organization for standardization (ISO) are not in good place therefore, these need to be addressed and actively managed.
Allergic responses to chemical exposure and other immunological skin condition among Nigerian laboratory university workers are worrisome. Many occupational chemical related workers in Nigerian laboratory universities have been injured and left in diverse health challenges [3]. The increase in absorption level of chemical exposure under the skin layers increases the risk and odd of being affected with CMH (Cellular mediated hypersensitivity), thus discomforting [4,5]
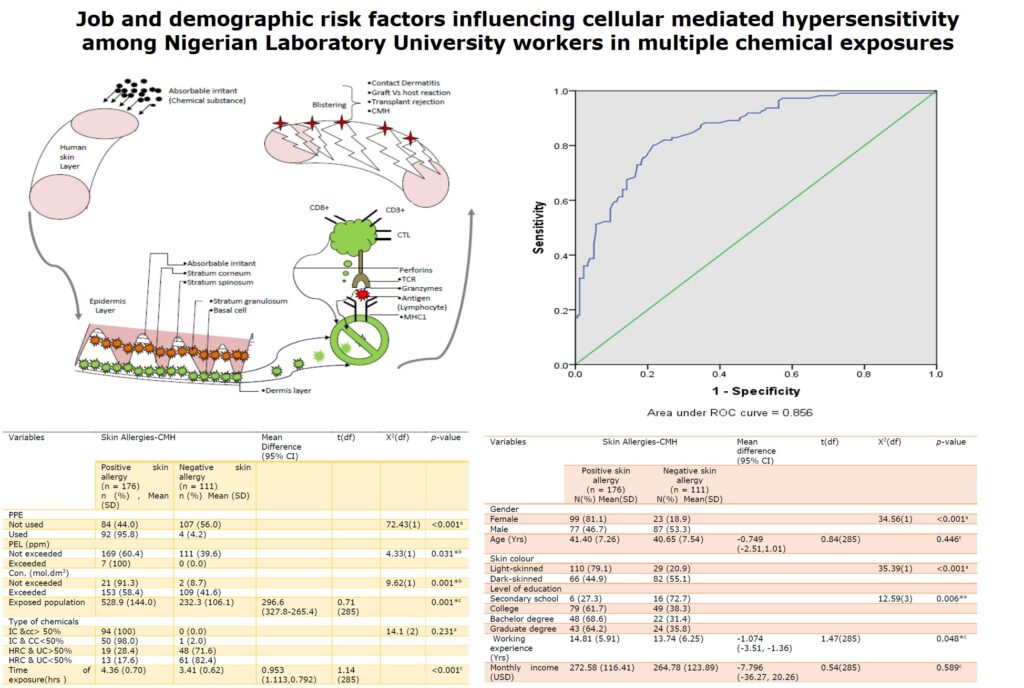
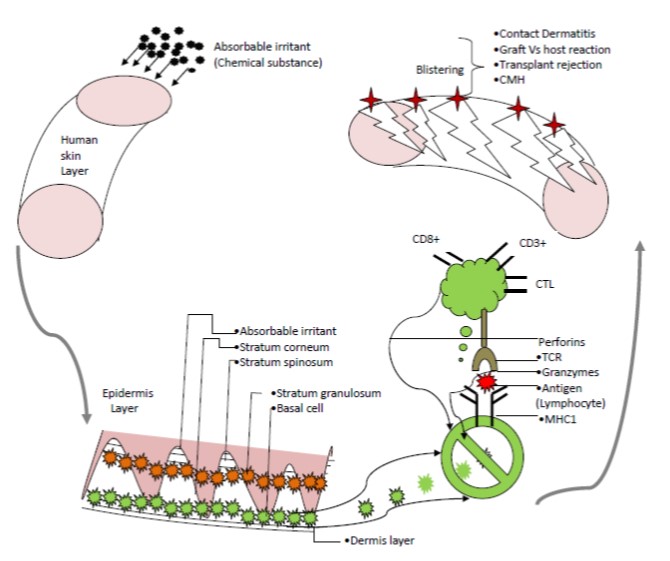
CMH is a sort of cell mediated cytotoxic reaction bound against human skin cells in an exposure to environment displaying foreign antigens onto to the cell surface proteins [5,6]. However, it is also believed that this chemo toxic is not so enough to initiate and propagate a reaction on its own under the skin layers due to the smallness of the chemical agent. Thus, it depends on the cell surface proteins for facilitation of the reaction to display and recognize the antigen by the appropriate T-cell[7]. In an exposure, the basal cells become swollen due to the presence of the absorbable chemicals under the skin layers and resultantly bind to the body proteins and start acts to look like an antigen or lymphocyte (The mechanism is summarized in Fig. 1. This therefore presents the fussy antigen onto the major histocompatibility complex (MHC) class one molecule for recognition. On the other hand, cytotoxic –T lymphocyte(CTL)becomes activated when it binds to antigen on top of the MHC1 by the T-cell receptor like manner with CD8+, and CD3+ cell surface proteins[8].Thus, leading to the periciliary layer of skin to detach and blisters and vesicles of erythema induced corresponding to CMH and other skin inflammatory condition are formed (tissue and cell damage) [9]. A study conducted in the North America by Warshaw et al. [10],showed that male sex have OR 0.59 (41%) less likely to develop CMH and other skin allergies compared to female. Survey studies, observations, and complaints revealed that workers spend much of their working time in chemical laboratories, hence being chemo-induced and have their skin inflamed due to immunological responses to the foreign and self-antigens from the skin surface [11,12] . National Institute of Science Laboratory Technology of Nigerian, physician experts in immunology, dermatology, occupational and environmental health and analytical chemists developed the operational definition for criteria required for a case of CMH that a chemical laboratory worker that report with chemo-induced injury and have erythema index difference (EID) ≥ 0.1 is described to have erythema inducement corresponding to CMH whereas EID <0.1 have no erythema inducement [13]. Hence the objective of this study was to determine the occupational and socio-demographic risk factors of the Nigerian laboratory university workers associated with CMH and erythema inducement in multiple chemical exposures
2.0 Materials and Methods
2.1 Inclusion and exclusion criteria
Those who were aged 18-year-old and above; and has been working at the same place for at least 2 years’ duration and active members of National Institute of Science laboratory technology of Nigerian were included in this study. Workers who have other chemical related occupations and or with genetic mutation (albinos) or receiving medication that can affect normal hemoglobin and melanin level were not included in this study. The final sample was drawn from a potential study population of 287 persons. Non-chemical laboratory worker volunteers with no history of skin allergies and erythema inducement and other immunological skin conditions were consented to participate in this study and were used as normal controls group and for purpose of research tools calibration.
2.2 Ethical approval
This study was conducted in accordance with the regulation and standard of Universiti Sains Malaysia (USM). Ethics approval of the current study was granted by Human Research Ethics Committee of USM (Ref.USM/JEPeM/16090130), National Health Research Ethics Committee (NHREC) of Nigerian (Ref.NHREC/01/01/2007-28/12/2016) as well as West African Bioethics and Collaborative Institutional Training Initiative (CITI) (Ref.ID: 5949144). All the protocols of the study were carried out in agreement with good research practice principle as enshrined in the Helsinki Declaration
2.3 Data collection
This was a cross sectional study conducted from November 2016 to May 2017 among 287 Nigerian laboratory university workers. The study area and the respondents were randomly selected from 30 available accredited Nigerian university laboratories. Erythema index meter was used to measure the allergic response corresponding to CMH. A brief structured demographic form was used to record the participants’ socio-demographic and occupational characteristics such as age, gender, working experience, and monthly income, personal protective equipment, permissible exposure limit and time of exposure to the chemical agent in the laboratory. The data were cleaned and screened for missing and erroneous entry prior to analyses. Computation of the results for socio-demographic and occupational data was executed in line with the International Contact Dermatitis Research Group (ICDRG) [14].Mean (SD) and frequency (%) were considered as descriptive analyses in this study. Also, Independent t-test was used to determine mean differences for the continuous variables, whereas the x2test was applied for descriptive statistics of frequency and percentage for sex, skin color, working experience, monthly income, educational level, personal protective equipment, permissible exposure limit and time of exposure to the chemical agent in the laboratory. Logistic regression (to estimate OR at 95% CI) was used for examining the associations between socio-demographic and occupational characteristics in the total study sample. First, a univariate logistic regression was applied. This was followed by multivariate logistic regression where the model significance was determined by the best selection procedure and the preliminary main effect model was processed using enter method. Alpha level of significance was set at (p<0.05) throughout the study. All the data analyses were done with Statistical Package for Social Science (SPSS) for Windows (IBM Inc., version 22.0).
2.3.1 Measurement tool
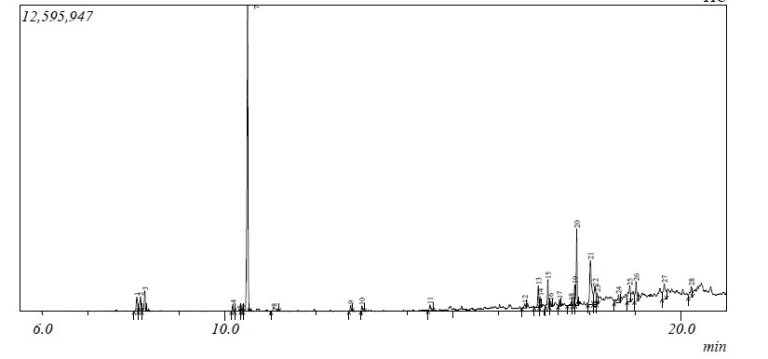
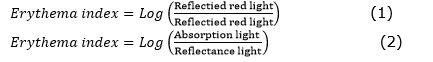
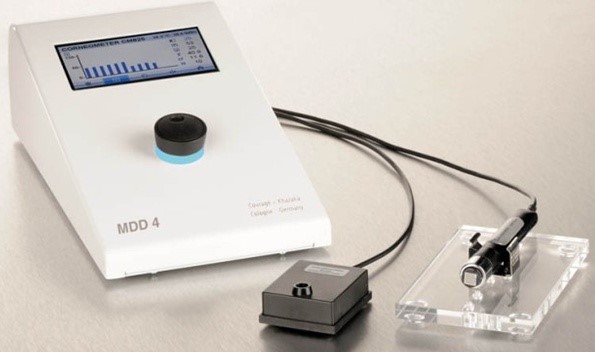
The allergic response was measured using erythema index meter (EIM) which is also known as MX18 [15,16] as seen in Fig. 2. The meter was calibrated and equipped with a probe to measure the chemo-induced skin injury corresponding to the erythema index (EI) of the participants in a susceptive environment using a measurement area of 4mm in diameter. EI in this study is defined as the threshold of epidermal damage that characterized the quantitative measurement of the biophysical characteristics of laboratory workers showing a positive reaction with CMH to chemical agent present under the skin layers from the surface. The erythema induced allergic response corresponding to EI was a measure of interaction to specular reflection of ultraviolet (UV) light that reveals optical properties of the skin cell with the hapten in an exposure. EI is said to be proportional to the length of exposure, types of substance, and concentration being dermal absorbed or physically contacted in a susceptive environment. The probe was pressed against the skin surface of the participating subjects to block outside light aiding proper revelation of the interaction. The measurement conducted on the workers prior to their work sessions in the laboratories (pre-exposure) represented a control group and after the work sessions (post-exposure) represent experimental group. With the MX18, light of two different wavelengths; one that is highly absorbed by hemoglobin while the other is highly reflected are emitted from a ring shaped light-emitting diode. Though, only light reflected from the skin layer of the subjects was recorded by the optical receiver. The absorption properties of both wavelengths are nearly the same. Thus, the induced erythema which is also described as EI in this study was obtained using ratio of the amount of reflected light while correlated with hemoglobin content as expressed in the equations below.
3.0 Results
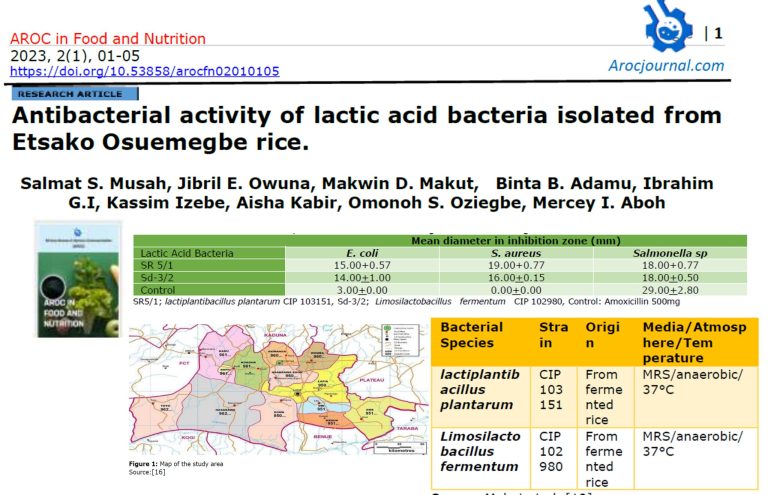
The study included 287 respondents. It was found that 176 out of 287 participants (61.3%) showed positive response to an allergic reaction whilst 99 (56.3%) of them were female. Three-quarter 110 (79.1) of the participants were light-skinned with positive CMH. Most of the respondents have a college education (61.7%) compared to other qualifications.
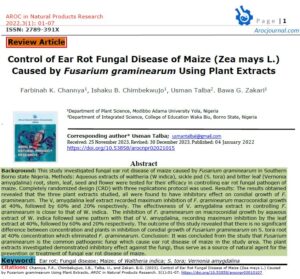
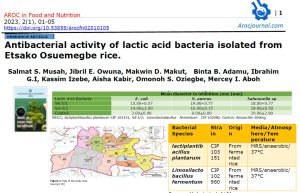
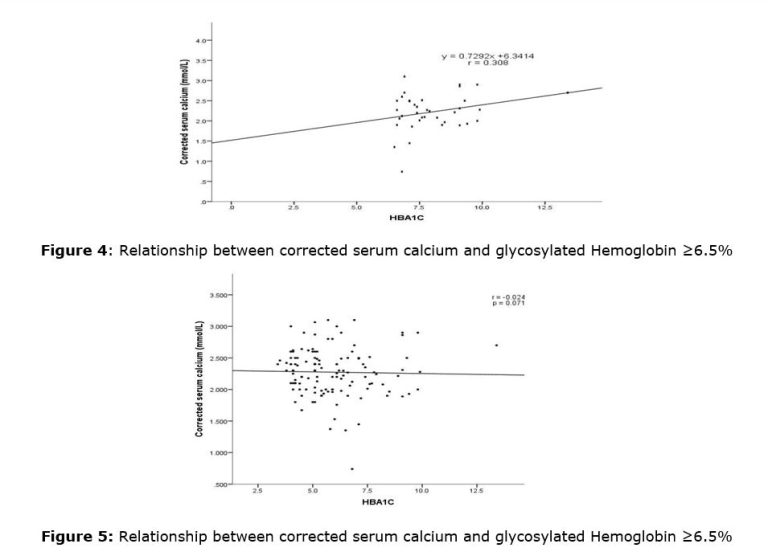
Correspondingly, the mean working experience was 14.81 (5.91) years. The x2test revealed that sex, skin color, working experience, educational level, personal protective equipment (PPE), permissible exposure limits (PEL), and time of exposure to the chemical agent (TOE) were significantly associated with positive CMH having p-value <0.001 for sex, skin color, PPE and TOE, p-value =0.004for educational level and p-value=0.001for PEL. The mean age and monthly income of the respondents was 41.1 (7.36) years and 272.6 (116.41) USD respectively. However, independent sample t-test indicated that working experience also has significant difference between these two groups with mean difference (95% CI) -1.074 (-3.51, -1.36) and p-value = 0.048 (Tables 1 and 2). In addition, the model stability and the diagnostic ability of the binary classifier showed in Fig. 3 were found to be 85.6% thus, showing the model to be fit.
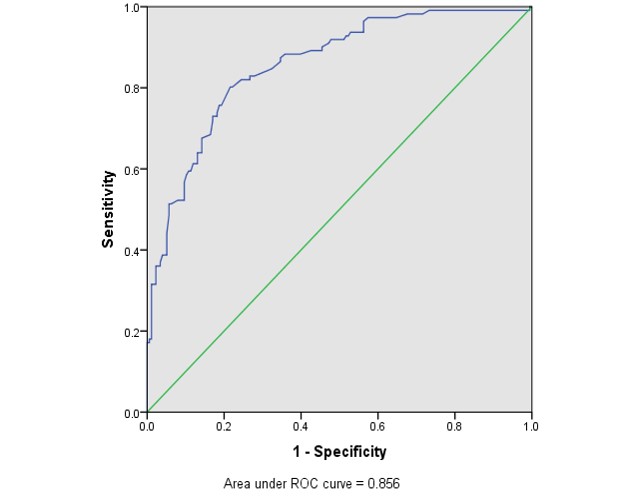
Table 1: Socio-demographic factors of skin allergies-CMH concerning investigated participants (n=287)
| Variables | Skin Allergies-CMH | Mean difference (95% CI) | t(df) | X2(df) | p-value | |
| Positive skin allergy (n = 176) N(%) Mean(SD) | Negative skin allergy (n = 111) N(%) Mean(SD) | |||||
| Gender | ||||||
| Female | 99 (81.1) | 23 (18.9) | 34.56(1) | <0.001a | ||
| Male | 77 (46.7) | 87 (53.3) | ||||
| Age (Yrs) | 41.40 (7.26) | 40.65 (7.54) | -0.749 (-2.51,1.01) | 0.84(285) | 0.446c | |
| Skin colour | ||||||
| Light-skinned | 110 (79.1) | 29 (20.9) | 35.39(1) | <0.001a | ||
| Dark-skinned | 66 (44.9) | 82 (55.1) | ||||
| Level of education | ||||||
| Secondary school | 6 (27.3) | 16 (72.7) | 12.59(3) | 0.006*a | ||
| College | 79 (61.7) | 49 (38.3) | ||||
| Bachelor degree | 48 (68.6) | 22 (31.4) | ||||
| Graduate degree | 43 (64.2) | 24 (35.8) | ||||
| Working experience (Yrs) | 14.81 (5.91) | 13.74 (6.25) | -1.074 (-3.51, -1.36) | 1.47(285) | 0.048*c | |
| Monthly income (USD) | 272.58 (116.41) | 264.78 (123.89) | -7.796 (-36.27, 20.26) | 0.54(285) | 0.589c |
aPearson’s Chi- Square test, bFisher’s Exact test, cIndependent –Sample T test. Criteria: Skin colour: visual interpretation, level of education: based on provided respondents’
Table 2: Occupational factors of skin allergies-CMH (n=287)
| Variables | Skin Allergies-CMH | Mean Difference (95% CI) | t(df) | X2(df) | p-value | |
| Positive skin allergy (n = 176) n (%) , Mean (SD) | Negative skin allergy (n = 111) n (%) Mean (SD) | |||||
| PPE | ||||||
| Not used | 84 (44.0) | 107 (56.0) | 72.43(1) | <0.001a | ||
| Used | 92 (95.8) | 4 (4.2) | ||||
| PEL (ppm) | ||||||
| Not exceeded | 169 (60.4) | 111 (39.6) | 4.33(1) | 0.031*b | ||
| Exceeded | 7 (100) | 0 (0.0) | ||||
| Con. (mol.dm3) | ||||||
| Not exceeded | 21 (91.3) | 2 (8.7) | 9.62(1) | 0.001*b | ||
| Exceeded | 153 (58.4) | 109 (41.6) | ||||
| Exposed population | 528.9 (144.0) | 232.3 (106.1) | 296.6 (327.8-265.4) | 0.71 (285) | 0.001*c | |
| Type of chemicals | ||||||
| IC &cc> 50% | 94 (100) | 0 (0.0) | 14.1 (2) | 0.231a | ||
| IC & CC<50% | 50 (98.0) | 1 (2.0) | ||||
| HRC & UC>50% | 19 (28.4) | 48 (71.6) | ||||
| HRC & UC<50% | 13 (17.6) | 61 (82.4) | ||||
| Time of exposure(hrs ) | 4.36 (0.70) | 3.41 (0.62) | 0.953 (1.113,0.792) | 1.14 (285) | <0.001c |
Table 3 shows the final model that was established following the necessary statistical tests. All the variables in the model were statistically significant with p-value less than 0.05. The variables that were retained in the multivariable logistic regression for association factors influencing CMH and the erythema inducement which were statistically significant include; sex, and skin color (p<0.001); educational level (p=0.049); personal protective equipment (p=0.011); permissible exposure limit (p=0.004); time of exposure to the chemical agent (p=0.001).
Table 3: Final model summary and associated factors for skin allergies-CMH (n=287)
| Variables | Simple Logistic Regression | Multiple Logistic Regression | ||||||
| B | LR/Wald | COR(95%Cl) | P-value | B | LR/Wald | AOR(95%Cl) | p-value | |
| Sex | ||||||||
| Female | 0 | 1 | 0 | 1 | ||||
| Male | -1.43 | 32.56 | 0.24 (0.12, 0.47) | <0.001 | -1.17 | 17.85 | 0.31 (0.12, 0.77) | 0.011 |
| Skin colour | ||||||||
| Light-skinned | 0 | 1 | 0 | 1 | ||||
| Dark-skinned | -1.54 | 33.32 | 0.24 (0.13, 0.36) | <0.001 | -1.07 | 13.42 | 0.49 (0.21, 0.81) | 0.001 |
| Level of education | ||||||||
| Secondary school | 0 | 1 | 0 | 1 | ||||
| College | 1.56 | 8.31 | 4.78 (1.65, 13.83) | 0.004 | 0.89 | 4.37 | 2.42 (1.10, 5.38) | 0.049 |
| Bachelor degree | 0.11 | 0.12 | 1.11 (0.60, 2.05) | 0.736 | 0.39 | 1.01 | 1.48 (0.69, 3.13) | 0.315 |
| Graduate degree | -0.19 | 0.29 | 0.82 (0.40, 1.67) | 0.587 | 0.012 | 0.03 | 1.01 (0.49, 2.68) | 0.476 |
| PPE | ||||||||
| Not used | 0 | 1 | 0 | 1 | ||||
| Used | -1.23 | 25.34 | 0.29 0.12, 0.97) | <0.001 | -0.91 | 18.24 | 0.40 (0.22, 0.77) | 0.001 |
| PEL (ppm) | ||||||||
| Not exceeded | 0 | 1 | 0 | 1 | ||||
| Exceeded | 1.16 | 9.11 | 3.29 (1.02,9.22) | 0.003* | 3.19 | 4.11 | 4.22 (2.88,12.11) | 0.004 |
| TOE(hours ) | ||||||||
| 2-3 | 0 | 1 | 0 | 1 | ||||
| 4-5 | 1.05 | 6.32 | 2.88 (1.00,7.11) | 0.001 | 2.01 | 3.55 | 3.11 (1.77,9.23) | 0.001 |
b= regression coefficient , AOT= Tim of exposure; PPE=Personal protective equipment; PEL=Permissible exposure limit, IC=Irritants chemical; ;CC=Corrosive chemicals; HRC=Highly reactive chemicals, UC=Unstable chemicals; SD=Standard deviation; PPM=part per million, PPE= Personal protective equipment; PEL= Permissible exposure limit; TOE=Time of exposure, COR= crude odds Ration, IC=Irritant chemicals; CC=Corrosive chemical; HRC=highly reactive chemicals, UC=Unstable chemicals; SD=Standard deviation; PPM=part per million, Cut-off points; PEL= CO=50ppm, CO2=500ppm, NO2=5ppm,SO2=5ppm,H2S=10ppm, Cut-off points; CWC= unitary value (1mol.dm3)
3.1 Discussion
The benefits of examining the relationship of occupational and socio-demographic risk factors of Nigerian laboratory university workers influencing CMH and erythema inducement in laboratory workers in multiple chemical exposures are being appreciated. Studies focused on types of chemical antigents responsible in chemo-induced skin injury have indicated nickel and sulphate as the major skin sensitizer [17,18]. In this study we found that occupational and socio-demographic characteristics revealing sex, skin color, working experience, educational level PPE, PEL, and time of exposure to the chemical agent were potential factors associated with the inducement of erythema corresponding to CMH. Multivariable analyses revealed the statistical significant factors associated with the inducement of erythema corresponding to CMH and hence were retained in the model as the main factors influencing the inducement of erythema corresponding to CMH in the university laboratory worker.
In the demographic and occupational characteristics, it was revealed that female sex, light- skinned, college educational level, working experience personal protective equipment, permissible exposure limits and time of exposure to the chemical agent (TOE) were potential risk factors associated with the development of CMH. Sex was reportedly an independently associated factor for CMH, contact dermatitis, and other occupational skin conditions among workers in the chemical related laboratory; typically female sex had the highest rate [19]. This study showed that male sex had likely significantly less odds of having CMH in accordance with findings by [10] with male found also had 69% less likely of developing CMH compared to female. The main reason was this might be due to high immunological responses to foreign and self-antigens in female plus constant use of skin care products and pieces of jewelry which considered being susceptive factors [20]. Additionally, psychological stress and constantly use of steroid cream might lead to superficial dilated blood vessels thus might be reflecting in the developing of CMH [21].
Likewise, skin color was revealed an exclusively significant associated predictor of CMH, contact dermatitis, and other occupational skin conditions among workers in the chemical related- job; typically light-skinned had the highest rate [22]. Chansky revealed in their studies that light–skinned is more susceptive to skin allergic reaction to chemical antigens as to dark-skinned 274(28.6) and 206(26.7). This study also shown that dark-skinned had likely significantly less odds of developing CMH compare to light which in conformity of Chansky’s documentation. Consequently, this might be due to a high concentration of melanin in dark-skinned diffuse and absorb the laser radiation of EIM hence, inhibiting light absorption to interact with the chemical hapten under the skin layer [23]. More so, physiological characteristics and existence of Langerhans cells on the surface of dark-skinned have been proven to be higher compared to light-skinned [24]. Thus, they help to protect the skin layers by keeping chemical antigens and other dangerous microbes from entering the body, hence reduce the chance of developing CMH [23,25].
Furthermore, the level of education was also an imperative significant associated factor for CMH and other skin allergic condition in occupational chemical related job reported by Peiser, Tralau, Heidler, Api, Arts, Basketter, English, Diepgen, Fuhlbrigge and Gaspari [5] and Weisshaar, et al. [26]. This study showed that college level of education had 2.42 times significantly higher odds of having CMH compared to other educational qualifications that were variables reference control. Correspondingly, this might suggest due to their role playing in the chemical laboratory as polytechnic graduates who is technically trained and sound for conduction of students’ practical and experiment, hence, exposed more and become susceptive to chemicals in the laboratories. Another prevalent reason could be the continuity of experience in chemical laboratory across the promotional stages and training which tends to be complex allows for a more uncomfortable and high stressful work environment [27,28]. Thus, the atmosphere somewhat becomes disruptive to them due to the constant flow of outside agents conducting research and observation, causing the workers leaving to another job [29]. This attitude induce psychological stress and depression in workers which might lead to superficial dilated of blood vessels and thus might increase the tendency of developing CMH [30].
Additionally, working experience shown an essential significant factor for CMH and other skin allergic disorder in chemical job-related investigated in other studies. The working experience more than 10 years reported by Lan, et al. [31]was 1.49 times higher odds of having occupational skin conditions and CMH related condition compared to the participants in other years of working experience categories. Thus, the present study revealed also the working experience 11-20 years had 1.58 times significantly higher odds of developing CMH compare to workers in other years of working experience categories that were variables reference control. In the same way, this might suggest due to fact that they are being considered as laboratory workforce as a result of their stable years of working experience thus, become more susceptive to the exposure [5,32]. In like manner, their role and position play in the chemical laboratory as intermediary technologists who always attain and administer practical for students, hence, turn out to be more susceptible to chemicals in the laboratories.
The proper use of the polymer of the ethylene vinyl alcohol co-polymerization laminated with polyethylene is probably the effective safety measure during a work session in a laboratory. Jeong, Kim, Park, Roh, Park and Lee [4]reported that an estimate of 30–45% of all cases of occupational diseases in the laboratories were due to inappropriate use of PPE whereas 10–15% laboratory workers used PPE properly during a work in the laboratories. This, report is supported by NIOSH and OSHA that lack of proper used of PPE might be associated with rise in the rate of skin allergic conditions and erythema inducement in the laboratory [33,34]. In this study, multivariate analysis showed that the workers who properly used PPE at the time of sampling had 60% less significant odds of been influenced with erythema inducement compared to those who did not.
PEL was reported by Kheur, et al. [35] as an independent factor with skin allergies; Skin biopsies analyzed for silver and related silver salt revealed a range of 0.03–13.48 ppm for the soluble group (median 0.115 ppm) and 0.03–0.77 ppm for the insoluble group (median 0.085 ppm). Thus, concluded that the silver concentrations found during work session exceeded 0.01 mg/m3 TLV set by NIOSH in the laboratories. However, this study reports multivariate analysis showing workers who were working with chemical mixture above the TVL (PLE exceeded) at the time of sampling had significantly higher odds of erythema inducement compare to the workers who had not exceeded TLV. This study defined PEL as method which has been developed to permit any chemical substance, no matter how toxic to be handled safely in a laboratory; this is done either by limiting the dose or controlling the exposure [36]. Thus, the high odd found in the findings could be due to the high probability that the chemical substance will cause harm under certain conditions if the chemicals exceed the PEL[37]. Another reason accounting for the high odds and disparity from within an established range from the previous studies might be due to the susceptibility of the biological system of the participants in a susceptive environment (the ability of a chemical substance to elicit a toxic response) [38].
In a study conducted in Germany by Geier, et al. [39], the trend of association with the duration of chemical allergen on the skin was revealed. The risk and effect of exposure were proportional to the duration of the exposure in the susceptive environment. Similarly, according to our findings, workers who spent 4-5hours working with chemical substances in laboratory at the time of sampling had 3.11 times significantly higher odds of been influenced with erythema inducement compare to those who spent 2-3 hours after controlling other variables. This finding could account for the fact that the toxic effects of chemical exposure depend on the amount, type, and length of time of exposure to the harmful substances, and most importantly, the severity account for long duration of exposures [38]. Many factors play a part in whether a subject will be affected with erythema inducement from being in contact with chemicals. For the discrepancy in the results, the reason could be attributed to the complex biological relationship existing among the subjects. Place of origin of the subjects, especially those from countries with high skin allergic prevalence is believed to contribute extensively.
5.0 Conclusions
Multiple regression analysis revealed that the CMH leading to erythema inducement was significantly associated and influenced by occupational and socio-demographic factors. Thus, they were the probable predictive risk factors associated with the CMH corresponding to erythema inducement in Nigerian laboratory university workers. Health education and adaptation programs should be conducted to minimize the chemo-induced skin injury among the workers. The trend of the results also suggest bad attitude to hazards and safety practice, poor laboratory procedures and practice, ineffective cleaning routine, and poor laboratory facilities.
Author’s Contributions Concept: Usaku Reuben design: Usaku Reuben and Godwin S. Abadi , definition of intellectual content Godwin S. Abadi: literature search: Micah M. Musa, clinical studies, experimental studies: Godwin S. Abadi:, software: Onyebuchi P. Uju, writing :Usaku Reuben, supervision: Usaku Reuben, funding acquisition: Godwin S. Abadi: data analysis:Usaku Reuben, statistical analysis, manuscript preparation: Usaku Reuben, manuscript editing and manuscript review: Onyebuchi P. Uju and Micah M. Musa .
Competing Interests: The authors have no conflict of interest in any form.
Funding: This research received no external funding”
Acknowledgements: This work was supported by University, Yola. The authors would like to give thanks to the support of the laboratory technologists of chemistry department, Modibbo Adama University, Yola. Thanks to all the participating chemical workers and other technologists in the sisters’ departments who provided assistance for our survey and collection of samples.
Ethics Approval Statement: Ethics approval of the current study was granted by Human Research Ethics Committee of USM(Ref.USM/JEPeM/16090130), National Health Research Ethics Committee (NHREC) of Nigerian (Ref.NHREC/01/01/2007-28/12/2016) as well as West African Bioethics and Collaborative Institutional Training Initiative (CITI) (Ref.ID: 5949144)
References
16. Miller, S.A.; Coelho, S.G.; Yamaguchi, Y.; Hearing, V.J.; Beer, J.Z.; de Gruijl, F. The Evaluation of Non‐invasive Measurements of Erythema as a Potential Surrogate for DNA Damage in Repetitively UV‐exposed Human Skin. Photochemistry and Photobiology 2017.
31. Lan, C.C.E.; Feng, W.W.; Lu, Y.W.; Wu, C.S.; Hung, S.T.; Hsu, H.Y.; Yu, H.S.; Ko, Y.C.; Lee, C.H.; Yang, Y.H. Hand eczema among University Hospital nursing staff: identification of high‐risk sector and impact on quality of life. Contact Dermatitis 2008, 59, 301-306.
32. Rietschel, R.L.; Fowler, J.F.; Fisher, A.A. Fisher’s contact dermatitis; PMPH-USA: 2008.
36. Watson, D. Occupational Safety and Health Administration. Green Technology 2011, 33, 3.6.